Inflammation is big business. With an aging population seeking to live a long and pain-free life, pharmaceutical companies are hard at work developing drugs to combat the many faces of inflammation. But this stuff isn't just for old folks – young bucks looking to get bigger and stronger can benefit as well.
Inflammation is the body's first response to an injury or infection. It was originally defined by the Latin words calor, dolor, rubor, and tumor, which mean heat, pain, redness, and swelling, respectively. What's interesting is the pain, redness, and swelling aren't directly caused by the infection or injury, but the immune system's response to them.
When an inflammatory response is triggered, chemical messengers called cytokines are released. This causes local dilation of blood capillaries and the skin to warm and redden due to increased blood flow to the area.
Dilation of the vasculature creates gaps between the endothelial cells lining the blood vessels, allowing blood plasma to leak into surrounding tissues. This expansion of fluid volume induces swelling, which leads to pain by putting more pressure on local nerve endings.
Cytokine release also makes vascular endothelial cells more "sticky," allowing white blood cells to attach and move from the blood into the inflamed tissue. To clear out any invading microorganisms and/or damaged tissue, white blood cells release substances that further increase inflammation and can cause local tissue damage, increasing pain.
While this all sounds like a very destructive process, acute inflammation is a normal part of life. The benefit of the temporary discomfort and swelling is that inflammation allows large numbers of immune cells to rapidly move into areas where they're needed to kill any invading microorganisms and begin the healing process.
For example, you're slicing your grass-fed flank into pieces to throw into a stir-fry and accidentally cut yourself. A blood clot rapidly forms to stop the blood loss, but the break in the protective barrier of your skin allowed bacteria in.
The immune system instantly keys up on the presence of these bacteria, triggering an inflammatory response. This makes blood vessels in the area "leaky," causing swelling, pain, and redness, but it also allows white cells to rapidly move into the area and kill the invading bacteria before they can spread and create a bigger infection.
The last thing we want to do is steer you away from training like an animal, so you should know that the inflammation that accompanies hard training is good.
In this case, muscular contractions cause a local increase in cytokines, activating inflammation. Think of cytokines as local chemical messengers – they're signaling proteins that help with intercellular communication, such as Interleukin 6 (IL-6) increasing muscle glucose uptake and the use of fats as fuel.
They also activate a local inflammatory response, kicking off a cascade of events associated with muscle growth and repair. Along with local growth factor release in response to mechanical tension, infiltrating immune cells play a direct role in satellite cell activation by locally releasing the cytokine TNFα.
Think of it like a construction site that's been damaged by a storm or hurricane. The foreman (cytokines) tells his crew to bring in more building supplies and to get busy fixing things – but now, make the building even more stable by using more material than what was originally planned. The result is a bigger and better building.
These types of acute inflammatory responses are totally normal and are involved in everything from wound healing to muscle growth. But what happens when inflammation is chronic instead of acute?
This is a big deal. The medical establishment tells us that hypertension is the "silent killer." According to many progressive doctors, chronic inflammation also deserves that designation.
Like acute or short-term stress, acute or local inflammation is usually okay. But chronic/low grade inflammation tends to be systemic, and can lead to joint stiffness and overall muscle aches and pain. At its most serious level, it can result in heart disease or insulin resistance, and most chronic degenerative diseases (think cardiovascular disease, various forms of arthritis, rhinitis) and even cancer are driven by chronic inflammation.
The bottom line is that chronic inflammation means loss of performance, and possibly even more serious health problems down the road.
Fat Balance
Most of us eat too much omega-6 fatty acids and not enough omega 3's. Here's why:
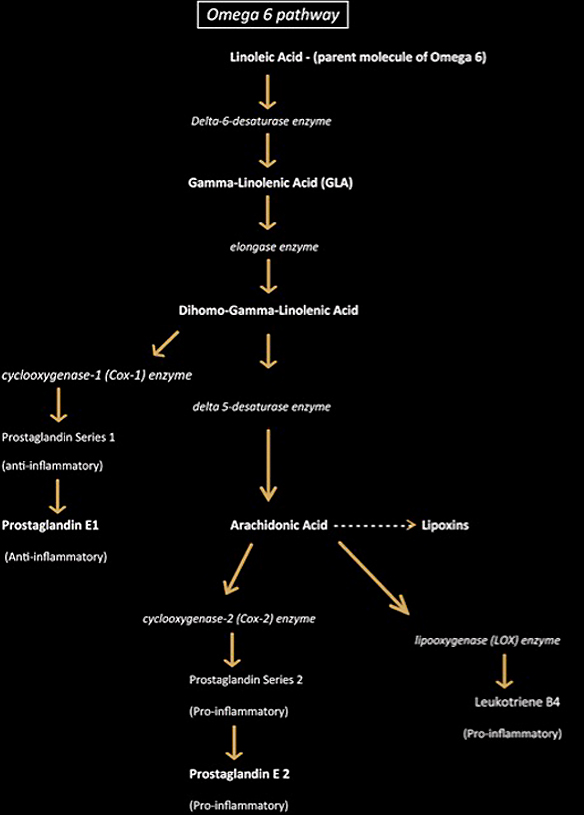
Competitive inhibition of delta-6-desaturase. Referring to the diagram below, you'll notice that the first step is dependent on delta-6-desaturase. When you take significantly more omega-3 than omega-6 – or vice versa – they compete against one another. This is why I tell people that super-loading omega-3 is not a good idea.
If you take in too much omega-3, you'll have issues converting omega-6, which is also essential. So don't fall for the "take 20-30 grams of fish oil a day" recommendations.
Fact is, some topnotch doctors report seeing patients with unusual bleeding and joint pain from taking excess omega-3. On the other hand, problems also occur with ingesting too much omega-6, which happens to be much more biologically active and will set the stage for more inflammation.
Here are some key points:
- Prostaglandins. These are lipid compounds derived from fatty acids. They can be both inflammation promoting and inflammation calming. An easy way to remember if the prostaglandin is anti- or pro-inflammatory (in case you're ever in a Jeopardy showdown) is that even numbers are pro-inflammatory, and odd numbers are anti-inflammatory.
- 'Ases.' Anything that ends in "ase" is an enzyme that pushes the conversion process along.
- Arachidonic acid isn't all bad. PG2 is created from AA, but so are lipoxins, powerful anti-inflammation agents. Lipoxins are a relatively new discovery, and help to slow down inflammation. They're produced if salicylic acid is available. So take a baby aspirin or eat plenty of fruits and veggies and you're set.
- Cox-1 production is good. Notice the pathway to the left of DGLA. This is a very strong anti-inflammatory pathway leading to PGE1. This is one reason why GLA is a very good thing.
Let's move on to the omega-3 pathway.

- The prostaglandins produced through this pathway are all anti-inflammatory.
- DHA also produces resolvins and protectins, and like lipoxins, are relatively new discoveries.
- Resolvins, as the name implies, resolves inflammation. Dr. Charles Serhan has done some fascinating work showing that Resolvin E (made from EPA) inhibited activation and movement of immune cells, resulting in diminished inflammation. It's also been shown to reduce skin inflammation, periodontal disease in animals, and other cool stuff. Resolvin D (made from DHA) has also shown tremendous benefit.
- Protectins, as the name implies, protects us in some way.
Trans Fats
Simply put, all trans fats are garbage. Look at the delta-6-desaturase enzyme in the two pathway diagrams. Trans fats can kill this step by inhibiting delta-6-desaturase. In other words, trans fats are crippling the healthy processing of fatty acids! Trans fats also get into your cell membranes and crowd out EFAs, thus increasing insulin resistance.
Alcohol
Just like trans fats, alcohol can slow delta-6-desaturase in its tracks. Alcoholics usually have chronic inflammation as a result. Go easy on the booze.
Insulin
I'm referring to insulin injections here. In some cases it may be a medical necessity, but for those injecting it for its anabolic properties, just know that it also fires up inflammation.
Excess Caffeine
Drinking a cup or two of coffee isn't a problem, but those who drink it all day are also increasing inflammation.
Excess Refined Carbs
Constantly slamming non-nutrient dense refined carbs can also create inflammation. One way is by making the delta-5-desaturase enzyme "hyperactive." On the omega-6 diagram you'll see that this is what converts DGLA to arachidonic acid, which produces inflammatory prostaglandins.
The most common way is to get a high sensitivity C-reactive protein test. Many physicians now use this test as a predictor for heart attack risk as well. Although not a perfect test, it's great for measuring low-grade chronic inflammation.
- A reading of less than 1 mg/L is low risk.
- A reading of 1 – 3 means is an average risk.
- A reading of 3 or above is high risk!
However, don't stop with the C-reactive protein test.
Next, get an omega-3 index test. Used to test for low omega-3, it's also being used as a measure for cardiac risk. I like the idea – instead of eliminating cholesterol through drugs, focus instead on raising omega-3 levels.
Ask your physician to measure your antioxidant levels as well. They can measure Vitamin A, E, and various minerals like selenium. Low antioxidant status usually means higher inflammation.
While I don't believe all anti-inflammatory drugs are evil, they are vastly overused and can be dangerous if abused. It's one thing to pop a few Motrin once a month to relieve soreness, but constant use can lead to trouble.
By inhibiting inflammatory prostaglandin activity, NSAIDs (non-steroidal anti-inflammatory drugs) may inhibit muscle protein synthesis after a workout. Also, NSAID junkies usually aren't aware that chronic NSAID use breaks down joint cartilage. Hello arthritis.
Conventional NSAIDs (such as Motrin, Naproxen, Advil, etc.) interfere with both cox-1 and cox-2. (Refer back to the diagram to see where they fall in the EFA pathways.) Cox-1 is essential for keeping a healthy stomach. In fact, helicobacter pylori infections that lead to ulcers are often caused by NSAIDs.
After the cox-2 enzyme was discovered, a new class of drugs was developed (Celebrex, Vioxx, Bextra) that suppress cox-2 but leave cox-1 alone. However, it was soon found that these cox-2 inhibitors also increased the risk of heart attack by four times compared to traditional NSAIDs.
- Balance EFA's. Dump any cooking oils made with corn, safflower, and other high omega-6 oils.
- Eat more cold-water fish or use fish oil capsules. Wild salmon, sardines, and herring are great sources as they're low in mercury, but if you still fear mercury, eat a serving of Brazil nuts every day. The selenium in them binds to mercury, making it nontoxic.
- Eat grass-fed meat. Pasture-raised, grass-fed livestock have superior fatty acid profiles. Just be careful here, this industry is full of bullshit artists. Get to know the farmer.
- Limit refined carbs. Refined sugars are anti-nutrients – they take more from your body than they give. They also raise insulin, which isn't catastrophic, but constantly doing so will result in increased inflammation. Use simple carbs post-workout only, and perhaps a small amount in your intra-workout shake. Alternatively, you can also use a carb-free protein hydrolysate like Mag-10® during training and forget the carbs altogether.
- Lose weight if overweight. Fat cells produce IL-6, TNFα, and other inflammatory cytokines. The fatter you are, the more you produce, and the more inflamed y
- Get a massage. A massage is an excellent way to relieve inflammation. Try to get one every week or two.ou get.
- Increase spices like curcumin, ginger, and oregano. Curcumin is a must. There are over 2000 studies supporting its use. It suppresses the interleukin-6 mentioned earlier, along with many other inflammation promoting compounds. I usually recommend ginger for those with upset stomachs or nausea. It also can block lipooxygenase. (See the omega-6 diagram for why that would be beneficial.)
- Avoid trans-fats. Nuff said.
- Avoid (or limit) alcohol. Hammering back shots like it's New Year's Eve is okay once in a while – like, say, on New Year's Eve – but if your idea of moderation is limiting alcohol consumption to just the days of the week that end in "y," then you probably have issues.
- Avoid excessive caffeine.
- Eat more fruits and veggies. This will increase the antioxidant status of your body.
- Use supplemental antioxidants and vitamins. If you can't get enough food in during the day, or simply don't like certain foods, use supplements. EPA/DHA and GLA supplements are number one, but you might also want to include vitamins A, C, E, and D.
Lastly, add in magnesium, selenium, and zinc.
Inflammation is a complex topic, and this article has merely scratched the surface. We hope that we've at least given you a few things to consider as you try to kick off 2012 on a healthier note. Remember, inflammation may be a "silent killer," but that doesn't mean you shouldn't take action.
- Maslinska D et al. Constitutive expression of cyclooxygenase-2 (COX-2) in developing brain. A. Choroid plexus in human fetuses. Folia Neuropathol. 1999 Jan 1;37(4):287-291
- Pedersen BK et al. Muscle as an endocrine organ: focus on muscle-derived interleukin-6. Physiol Rev. 2008 Oct;88(4):1379-406.
- Palacios D et al. TNF/p38α/Polycomb Signaling to Pax7 Locus in Satellite Cells Links Inflammation to the Epigenetic Control of Muscle Regeneration Cell Stem Cell. 2010 Oct 8;7(4):455-69.
- Rashad S et al. Walker F. Effect of non-steroidal anti-inflammatory drugs on the course of osteoarthritis. Lancet. 1989 Nov 11;2(8672):1149.
- Teather LA et al. Post-training cyclooxygenase-2 (COX-2) inhibition impairs memory consolidation. Learn Mem. 2002 Jan;9(1):41-7.
- Trappe TA et al. Effect of ibuprofen and acetaminophen on postexercise muscle protein synthesis. Am J Physiol Endocrinol Metab. 2002 Mar;282(3):E551-E556.
- Vazquez-Vela ME et al. White adipose tissue as endocrine organ and its role in obesity. Arch Med Res. 2008 Nov;39(8):715-28.





