The Truth About Exogenous Ketones
Ketones are all the rage among low carbers. And like most things in nutrition and performance, we've found a way to get them in supplement form so we don't have to do any actual work.
What are ketones? They're a byproduct of ketosis caused by the process of converting fat to fuel. Your body makes them when it's in a calorie or carb restricted state. What do they do? The body and brain can use them as fuel without the presence of glucose in the blood.
And now, you can take ketone supplements (salts and esters), known as exogenous ketones, without actually restricting anything. According to those promoting this nasty-tasting supplement, that means you can have a brain and body fuelled by ketones, along with all of the supposed health benefits that come with running on fat. Well, don't fall for it.
Exogenous Ketones = Endogenous Fat Storage?
The problem with ketone supplementation (EXOgenous) is that it's not even close to the same thing as being in ketosis (ENDOgenous ketone production). And just like the butter-blended-into-coffee trend, it's a farce.
Ketones may be depressing dieters' hunger and giving them a hit of energy and cognitive enhancement, but it's INHIBITING their ability to burn fat, providing zero nourishment, and doing nothing for their metabolic health. There's an assortment of evidence suggesting that it's probably making things worse.
Think of exogenous ketones kind of like alcohol. When they're consumed, everything is stored and nothing else is burned. So any lipolysis (fat burning) that would be taking place is halted; any glucose and fatty acids in your blood that were circulating are stored; and the ingested ketones are burned until there aren't any left.
More importantly, this clearance of alternative fuels (glucose and fatty acids) appears to be driven by insulin. Even though some have suggested the ketones facilitate an increase in glucose uptake (via pyruvate dehydrogenase activation), it's pretty clear that they facilitate an increase in insulin.
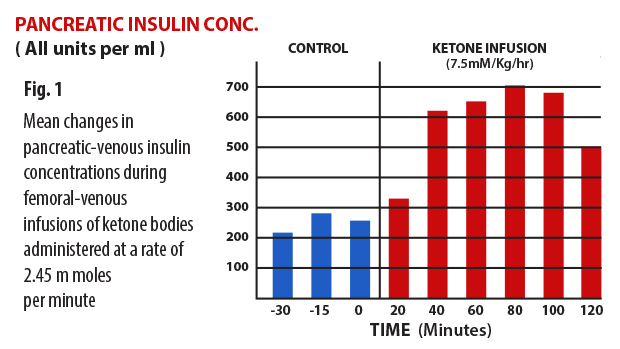
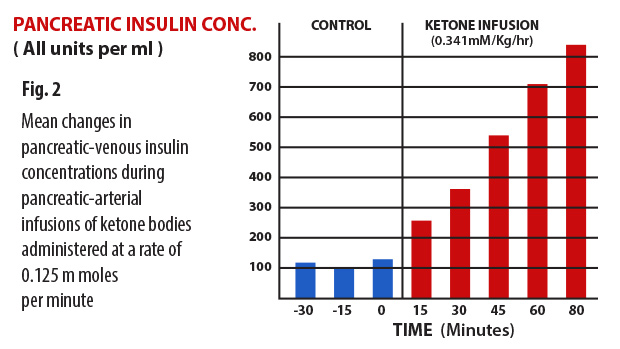
Figure 1-2: The data demonstrate that the pancreatic beta cells respond to hyperketonemia, induced by infusions of β-hydroxybutyrate and acetoacetate, with an increased rate of insulin secretion that is immediate in onset and significant in amount.
So unless you're in a fasted state or dieting, you need to ask yourself whether ketones are enhancing your performance to the point where storing fat and carbs, exiting fat burning mode, and secreting insulin is worth it. And if you are fasted or dieting, you need to ask yourself, "What's my goal?"
Ketones and Fat Loss
Most people restricting carbs, or intermittent fasting to get into ketosis, are doing it to burn fat and get lean. So it's counterproductive to ingest ketones that will inhibit that process. Especially when we have brain boosters like caffeine that will enhance it.
And remember, the process of creating ketones in the body requires energy, while ingesting exogenous ketones requires none. If fat loss is the goal, why wouldn't you want your body to do the work of producing its own energy source (ketones)?
There is one viable explanation for consuming ketones. If you're in a calorie or carb-restricted state, then maybe during a workout it would make sense. But even then, that really only applies to endurance activities, since it has more to do with enhancing aerobic performance (where oxygen is required), than it does with enhancing high-intensity efforts (where it's not).
In animal studies, those supplementing exogenous ketones (beta-hydroxybutyrate) generated more ATP (energy) per unit of oxygen compared to glucose or fatty acids.
The lifter is relying on glycogen (not fat), and his or her workout is already enhancing the ketotic-state, so it seems the creatine (fuels ATP-PC) and carb-cycling (fuels glycolysis) they're already doing makes a lot more sense than the ketones (fuels oxidation).
Ketones and Health
For those who are already lean and choose to fast or diet for long-term health, it's a bit of a different story. Although the question becomes: Will exogenous ketones do more for you than endogenous ketones?
Some think so because higher ketone levels imply increased fuel for the brain and heart (that prefer ketones), and increased protection against inflammation and oxidation. But are the health benefits coming from the ketones themselves, or are they coming from the state you have to put your body in to actually produce them? And if you're kicking yourself out of ketosis by ingesting ketones would you still get the same benefits?
The answer to both questions is no. The following benefits of ketosis aren't attributable to ketones:
- Upregulation of glutathione (an antioxidant)
- Removal of dead and damaged cells (autophagy)
- Elevation of NAD+ and other beneficial metabolites
- Activation of life-extending enzymes (ilke sirtuin)
- Reduction in amyloid-beta (plaque) in the brain
- Improvement in ketone and glucose transport and delivery (GLUT-1)
- Enhancement in mitochondrial function
- Increased AMP-activated protein kinase activation (AMPK)
- Reduced insulin and IGF-1 signaling
And that's before getting into the fact that adding ketones to a mixed diet creates an energy surplus, and non-glucose utilizing state, which doesn't bode well for cancer prevention since it seems to have more to do with energy and glucose deprivation, fatty-acid utilization, and healthy mitochondria.
Likewise, insulin sensitivity and cardiometabolic health are improved drastically during nutritional ketosis, while supplemental ketones have no impact here other than supplying an alternative fuel source to glucose and potentially reducing inflammation.
The Good, Bad, and Ugly
It's not all bad when it comes to exogenous ketones. For anyone with Parkinson's, Alzheimer's, epilepsy, ALS, Huntington's, brain cancer or any other degenerative neurological condition, they might be life-changing.
And for the aerobic athlete, they can provide an additional fuel source outside of dietary carbohydrates and fat – giving the carbed-up competitor the ability to go further before having to refuel, and the fat-adapted competitor the ability to go further before tapping into their personal reserves.
But suggesting individuals already fasting, restricting calories, or cutting carbs will get anything other than a brain buzz is misleading. And to serve up exogenous ketones to an obese, insulin-resistant general population with promises of fat-burning and disease prevention is potentially damaging.
Sure, it might suppress hunger and give a damaged brain a useable fuel source, but what happens when pre-diabetic Pete starts adding ketones to his glucose-rich blood? Or anaerobic Andy continues reloading with the same amount of carbs post-workout even though the liver glycogen he normally burns during his sessions is now suppressed?
Ketones may be a better source of fuel than glucose, and a far better beverage than Fruitopia, but it's a question of whether or not you can spare the extra fuel. Because just like adding sugar to a diet, it's like pressing pause on the fat burning process since the body preferentially burns it for fuel. Adding ketones to the diet does the same thing.
And if you know your science, then what that extra dose of ketones leads to is glycation, oxidation, and conversion to fat for the metabolically deranged majority, and elevated insulin because of excess energy in the bloodstream.
A Better Approach
Fix your diet and get into actual ketosis if that's your goal. But again, that would require your body to do some actual work.
References
- Manninen AH. 2004. Metabolic Effects of the Very-Low-Carbohydrate Diets: Misunderstood "Villains" of Human Metabolism. J Inter Soc Sport Nutr 1:7.
- Bjorntorp P, and Schersten T. 1967. Effect of beta-hydroxybutyrate on lipid mobilization. Am J Physiol. 212(3):683-7.
- Taggart AK, et al. 2005. (D)-beta-Hydroxybutyrate inhibits adipocyte lipolysis via the nicotinic acid receptor PUMA-G. J Biol Chem 280(29):26649-52.
- Stubbs BJ, et al. 2015. Concomitant meal ingestion alters levels of circulating ketone bodies following ketone ester drinnk [Abstract]. Proc Physiol Soc 34, PC235
- Fery F and Balasse EO. 1988. Effect of exercise on the disposal of infused ketone bodies in humans. J Clin Endocrinol Metab 67(2):245-50.
- Madison LL, et al. 1964. The hypoglycemic action of ketones. II. Evidence for a stimulatory feedback of ketones on the pancreatic beta cells. J Clin Invest 43(3):408-15.
- Robinson AM and Williamson DH. 1980. Physiological roles of ketone bodies as substrates and signals in mammalian tissues. Physiol Rev 60(1):143-87.
- Balasse EO, et al. 1970. Evidence for a stimulatory effect of ketone bodies on insulin secretion in man. Horm Metab Res 2(6):371-2.
- Owen OE, et al. 1973. Rapid intravenous sodium acetoacetate infusion in man. Metabolic and kinetic responses. J Clin Invest. 52(10):2606-16.
- Fery F, et al. 1982. Hormonal and metabolic changes induced by an isocaloric isoproteinic ketogenic diet in healthy subjects. Diabete Metab 8(4):299-305.
- Langfort J, et al. 1996. Effect of low-carbohydrate-ketogenic diet on metabolic and hormonal responses to graded exercise in men. J Physiol Pharmacol 47(2):361-71.
- Cahill GF Jr and Veech RL. 2003. Ketoacids? Good medicine? Trans Am Clin Climatol Assoc 114:149-163.
- Koeslag JH, et al. 1980. Post-exercise ketosis. J Physiol 301:79-90.
- Phinney SD. 2004. Ketogenic diets and physical performance. Nutr Metab 1:2.
- Singh N, et al. 2014. Activation of Gpr109a, Receptor for Niacin and the Commensal Metabolite Butyrate, Suppresses Colonic Inflammation and Carcinogenesis. Immunity 40(10):128-136.
- Shimazu T, et al. 2013. Suppression of oxidative stress by beta-hydroxybutyrate, an endogenous histone deacetylase inhibitor. Science 339:211-214.
- Newman JC and Verdin E. 2014. Ketone bodies as signaling metabolites. Trends Endocrinol Metab. 25(1):42-52.
- Jarrett SG, et al. 2008. The ketogenic diet increases mitochondrial glutathione levels. J Neurochem 106(3):1044-51.
- Ziegler DR, et al. 2003. Ketogenic Diet Increases Glutathione Peroxidase Activity in Rat Hippocampus. Neurochem Res 28(12):1793-1797.
- Furuya N, et al. 2004. Autophagy and cancer. In Autophagy. D.J. Klionsky editor. Landes Bioscience. Georgetown, Texas, USA. 244-253.
- Houtkooper RH, et al. 2010. The Secret Life of NAD+: An Old Metabolite Controlling New Metabolic Signaling Pathways. Endocr Rev 31(2):194-223.
- Stein LR and Imai S. 2012. The dynamic regulation of NAD metabolism in mitochondria. Trends Endocrinol Metab 23:420-428.
- Srivastava S, et al. 2013. A ketogenic diet increases brown adipose tissue mitochondrial proteins and UCP1 levels in mice. IUBMB Life 65:58-66.
- Van der Auwera I, et al. 2005. A ketogenic diet reduces amyloid beta 40 and 42 in a mouse model of Alzheimer's disease. Nutr Metab 2:28.
- Puchowicz MA, et al. 2007. Diet-induced ketosis increases capillary density without altered blood blow in rat brain. Am J Physiol Endocrinol Metab 292:E1607-E1615.
- Jornayvaz FR, et al. 2010. A high-fat, ketogenic diet causes hepatic insulin resistance in mice, despite increasing energy expenditure and preventing weight gain. Am J Physiol Endocrinol Metab 299:E808-815.
- Kennedy AR, et al. 2007. A high-fat, ketogenic diet induces a unique metabolic state in mice. Am J Physiol Endocrinol Metab 292:E1724-1739.
- Kinzig KP, et al. 2010. Insulin sensitivity and glucose tolerance are altered by maintenance on a ketogenic diet. Endocrinology 151:3105-3114.
- Freedland SJ, et al. 2008. Carbohydrate restriction, prostate cancer growth, and the insulin-like growth factor axis. Prostate 68:11-19.
- McDaniel SS, et al. 2011. The ketogenic diet inhibits the mammalian target of rapamycin (mTOR) pathway. Epilepsia 52:e7-11.
- Warburg O, et al. 1927. The metabolism of tumors in the body. J Gen Physiol 8:519-530.
- Hanahan D and Weinberg RA. 2011. Hallmarks of cancer: the next generation. Cell 144: 646-674.
- Mobbs CV, et al. 2007. Secrets of the lac operon. Glucose hysteresis as a mechanism in dietary restriction, aging and disease. Interdiscip Top Gerontol 35:39-68.
- Warburg O. 1956. On respiratory impairment in cancer cells. Science 124: 269-270.
- Pelicano H, et al. 2006. Mitochondrial respiration defects in cancer cells cause activation of akt survival pathway through a redox-mediated mechanism. J Cell Biol 175: 913-923.
- Paoli A, et al. 2013. Beyond weight loss: a review of the therapeutic uses of very-low-carbohydrate (ketogenic) diets. Eur J Clin Nutr 67, 789-796
- Westman EC, et al. 2008. The effect of a low-carbohydrate, ketogenic diet versus a low-glycemic index diet on glycemic control in type 2 diabetes mellitus. Nutr Metab 5:36.
- Santos FL, et al. 2012. Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev 13(11):1048-1066.
- Hickey JT, et al. 2003. Clinical use of a carbohydrate-restricted diet to treat the dyslipidemia of the metabolic syndrome. Metab Syndr Relat Disord 1(3):227-32.
- Youm YH, et al. 2015. The ketone metabolite β-hydroxybutyrate blocks NLRP3 inflammasome-mediated inflammatory disease. Nat Med 21(3):263-9.
- Reger MA, et al. 2004. Effects of beta-hydroxybutyrate on cognition in memory-impaired adults. Neurobiol Ag 25(3):311-4.
- Baranano KW and Hartman AL. 2008. The Ketogenic Diet: Uses in Epilepsy and Other Neurologic Illnesses. Curr Treat Options Neurol 10(6): 410-419.
- Zhao Z, et al. 2006. A ketogenic diet as a potential novel therapeutic intervention in amyotrophic lateral sclerosis. BMC Neurosci 7:29.
- Sadri-Vakili G and Cha JH. 2006. Mechanisms of disease: Histone modifications in Huntington's disease. Nat Clin Pract Neurol 2:330-338.
- Gasior M, et al. 2006. Neuroprotective and disease-modifying effects of the ketogenic diet. Behav Pharmacol 17(5-6):431-439.
- Veech RL, et al. 2001. Ketone bodies, potential therapeutic uses. IUBMB Life 51(4):241-7.
- Veech RL. 2004. The therapeutic implications of ketone bodies: the effects of ketone bodies in pathological conditions: ketosis, ketogenic diet, redox states, insulin resistance, and mitochondrial metabolism. Prostaglandins Leukot Essent Fatty Acids 70(3):309-19.
- Hashim SA and VanItallie TB. 2014. Ketone body therapy: from the ketogenic diet to the oral administration of ketone ester. J Lipid Res 55(9):1818-26.
- Ebert TR, et al. 2007. Fluid and food intake during professional men's and women's road-cycling tours. Int J Sports Physiol Perform 2(1):58-71.
- Cox PJ, et al. Nutritional Ketosis Alters Fuel Preference and Thereby Endurance Performance in Athletes. Cell Metab 24(2):256-258.
- Cox PJ and Clarke K. 2014. Acute nutritional ketosis: implications for exercise performance and metabolism. Extrem Physiol Med 3:17.